Introduction to Breast Imaging
Debra Somers Copit, MD, FACR
Director, Breast Imaging
Einstein Healthcare Network
Associate Professor Radiology, Sidney Kimmel MedicalCollege of Thomas Jefferson University

Conference Rules!
•Take notes
•Study your notes the night before
•Try to keep your eyes open
•Don’t be afraid to answer a question

Conference Curriculum
•Introduction/overview of mammography
•Introduction/overview of breast ultrasound
•Breast pathology
•Mammographic technique/physics
•MQSA, ACR requirements,QC, digital artifacts
•Post operative breast
•Digital breast tomosynthesis
•The male breast
•Systemic diseases on breast imaging
•High risk lesions/managing the high risk patient

What Does Breast Imaging Involve?
•Mammography (screening, diagnositic,tomosynthesis)
•Ultrasound
•MRI
•Stereotactic & ultrasound guided biopsy
•Ductography
•Cyst aspiration
•Contrast enhanced mammography
•BSGI

Estimated US Cancer Cases*
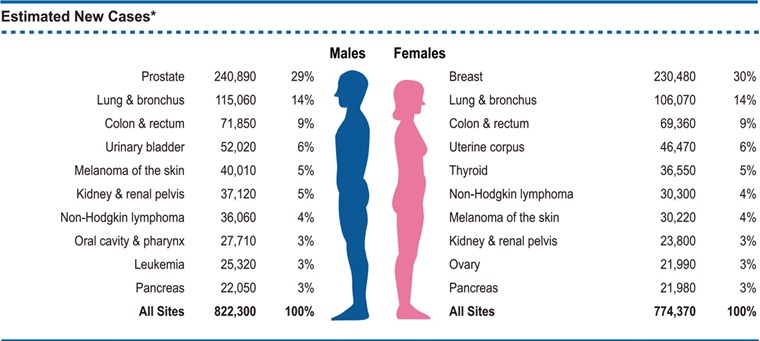
*CA Cancer J Clin 2011

Estimated Cancer Deaths*
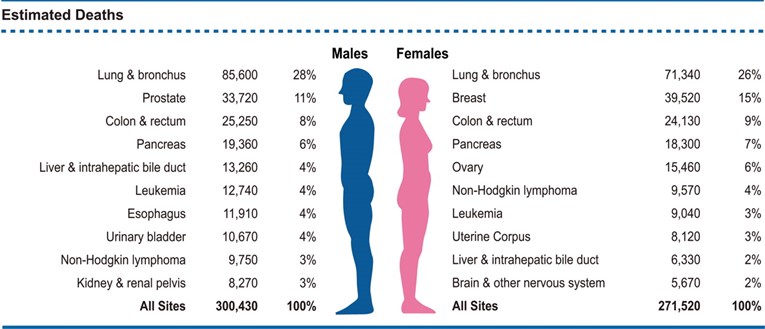
*CA Cancer J Clin 2011

Probability of Invasive Breast Cancerby Age
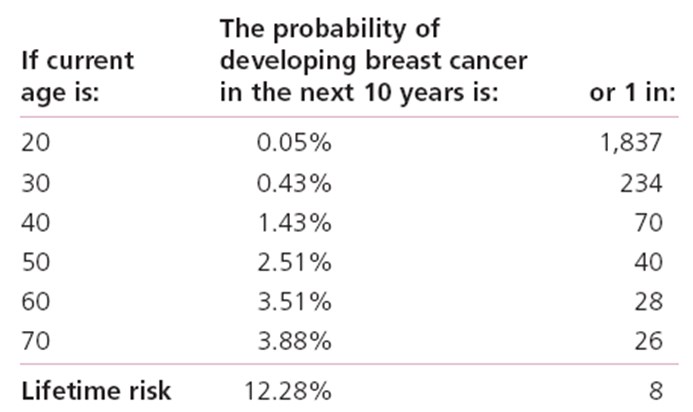
American Cancer Society Surveillance Research, 2007

Risk Factors
Epidemiologic
•Early menarche
•Late menopause
•Family history
•Personal history
•Female gender
•Prior chest radiationbetween 10-30 yrs
Histologic
•Atypical lobularhyperplasia
•Atypical ductalhyperplasia
•Lobular carcinoma in situ
•?radial scar
•?papillomatosis

Relative Risk
First degree relative with breast cancer 2X
Personal history of breast cancer 4-5X
Biopsy revealing ADH, ALH 5X
Biopsy revealing LCIS 10X
Radiation for Hodgkins 20-30 yrs 7X
Radiation for Hodgkins <20 yrs 56X
BRCA 1 or 2 mutation 40-85X

Staging(TNM) & Survival
Stage
•0
•I
•IIA
•IIB
•IIIA
•IIIB
•IIIC
•IV
5-year Survival Rate
•93%
•88%
•81%
•74%
•67%
•41%
•49%
•15%

Stage Distribution and 5-year RelativeSurvival by Stage at Diagnosis2001-2007
Stage at Diagnosis Stage 5- year Relative Distribution (%) Survival
Localized 60 98.6
(confined to primary site)
Regional 33 83.8
(spread to regional nodes)
Distant 5 23.4
(cancer has metastasized)
Unknown 2 52.4
(unstaged)

SEER Cancer Statistics Review, 1975-2008, National Cancer Institute. Bethesda, MD,http://seer.cancer.gov/csr/1975_2008/, based on November 2010 SEER data submission

SCREENING Mammography: WhyDoes It Work?
•Inexpensive
•Widely available
•Non-invasive
•Reduces mortality

How Do We Know If ScreeningMammography Is Efficacious
•Goal 1: detect breast cancer at a smaller size and earlier stagethan without the test (Breast Cancer Detection Demonstration Project[3])
•Goal 2: leads to a statistically significant reduction in mortality
(7 RCTs of mammography screening [4])
•Goal 3: When the screening test is introduced into the generalpopulation, the death rate declines
30% reduction in mortality from breast cancer in U.S. once screening widelyutilized

How Screening Meets These Goals:Other Evidence
•Breast cancers found by screening: mediansize 1.0-1.5 cm [5]
•Breast cancers found by clinical breastexamination (CBE) or by a woman herself:median size 2.0-2.5 cm [5]
•Node positivity:
~10% of invasive cancers < 1cm
~35% of those < 2 cm
~ 60% > 4 cm [6]

Lead Time & Selection Bias
•Cancer detection by screening will bias resultsin favor of screening regardless of whether ornot the natural history of the disease has beenaltered (lead time bias)
•Women who participate in screenings may behealthier than those who do not (selectionbias)

Randomized, controlled trials:invited group & control group
•Having these 2 groups: invited group andcontrol group-corrects for lead time andselection bias
•HIP (Health Insurance Plan of NY) Trial was thefirst in 1960s, 8 more trials have followed
•All have shown fewer breast cancer deaths inthe screened vs control group

Randomized, controlled trials:compliance and contamination
•Data from noncompliant women included (women ininvited group who die from breast cancer eventhough they were not screened by choice)
• contamination (women in control group who did notdie from breast cancer because they chose to bescreened outside the trial)
•At best only 70% of invited women participate
•Lack of complete participation combined withcontamination and non-compliance means that theRCTs underestimate the benefit of screening

What are the negatives of amammogram?
For every 1000 women screened
•80-100 called back
•45-65 of those recalled will be normal(“falsepositive”)
•20 asked to return in six months ( less than a2% chance of being cancer)
•15 will have a biopsy recommended, of which2-5 will have cancer and 10-13 will be negative(false positive) [18]

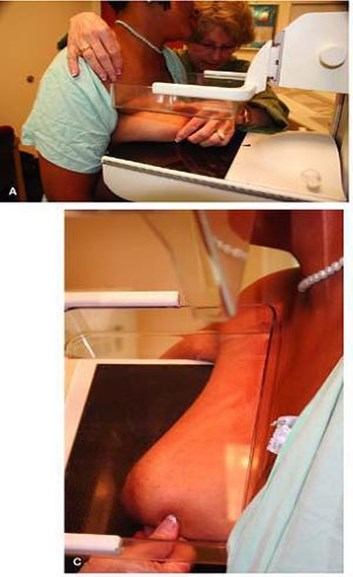
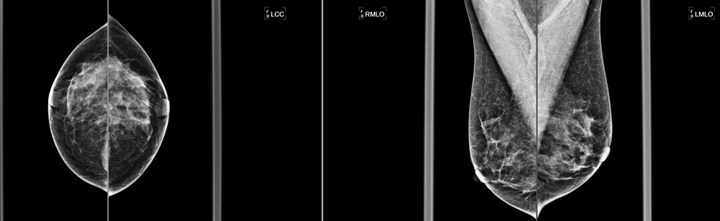
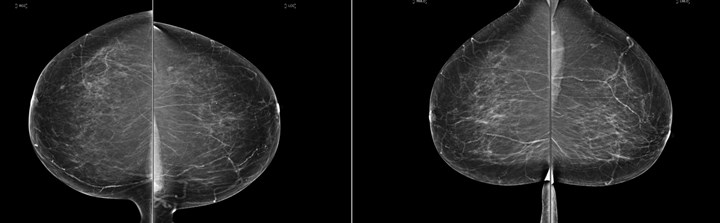
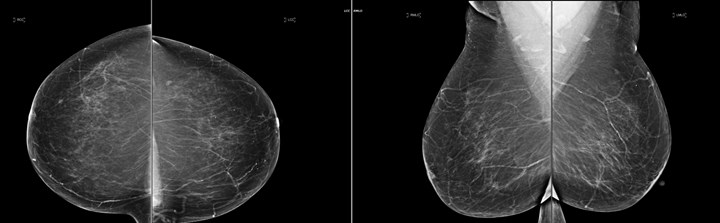
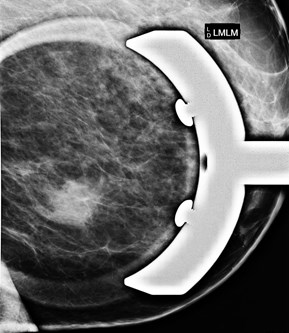
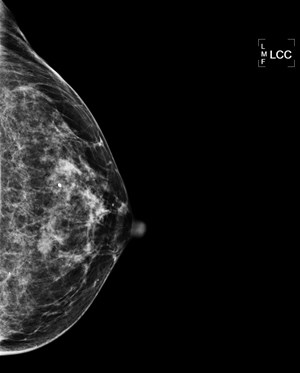
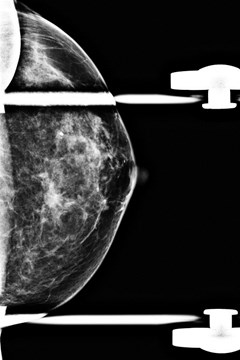
Positioning for craniocaudalview
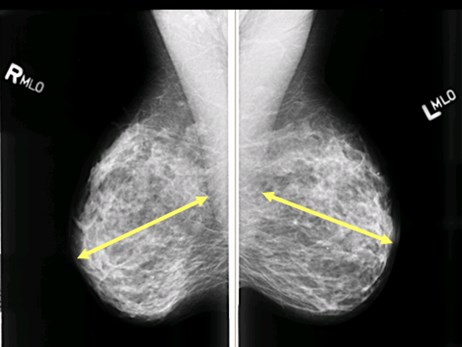
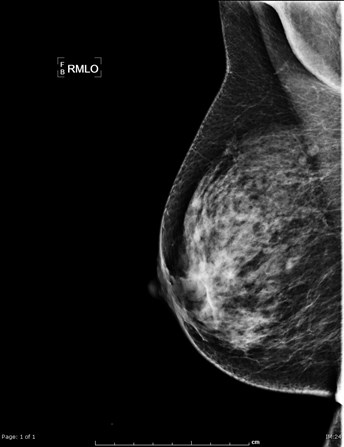
Positioning formediolateral oblique view



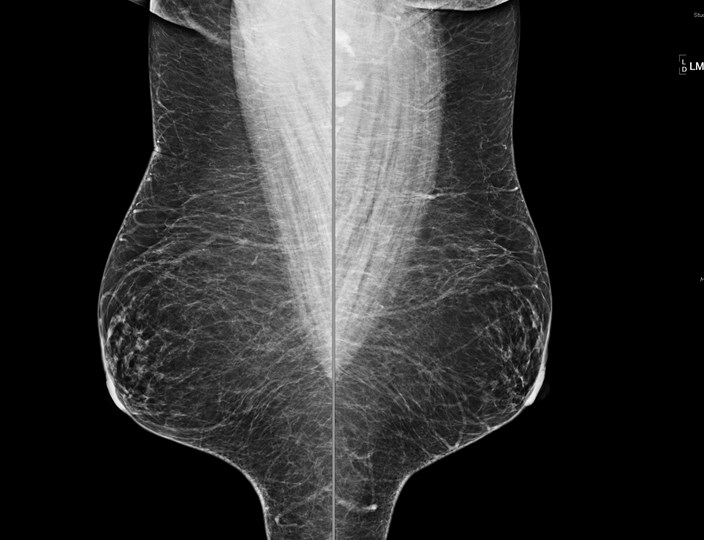

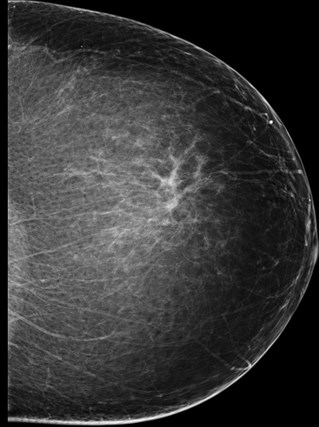
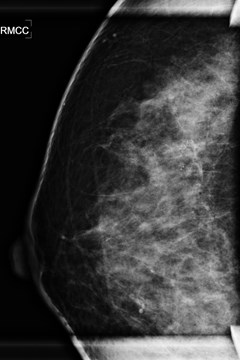
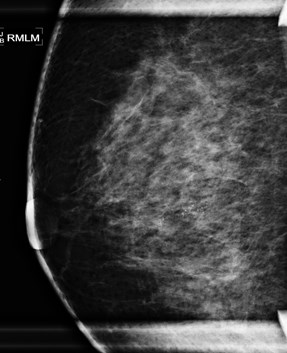
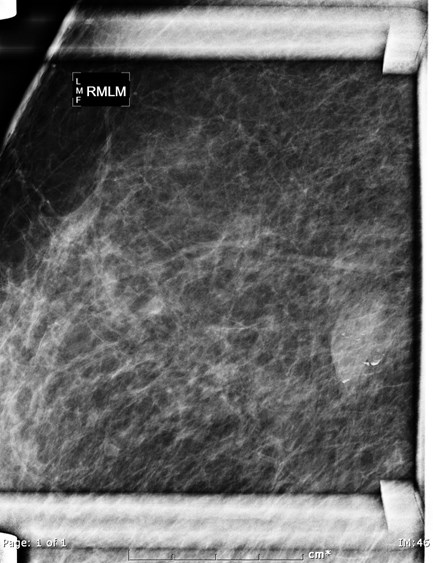
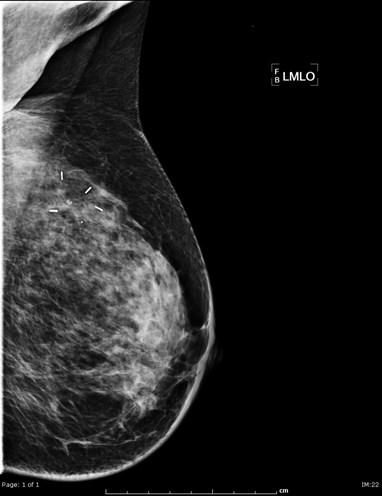
Mammographic Technique: TheMLO view
•Angle used depends on angle of pectoralis muscle(usually between 45 and 60 degrees)
•Pectoralis muscle should be seen down to the levelof the nipple 90% of time
•Muscle border should be convex
•Inframammary fold (IMF) should be open
•Posterior nipple line (aka nipple axis line)-drawn fromnipple to pec used to determine adequacy of CC view

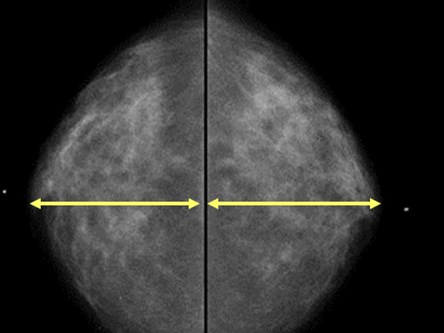
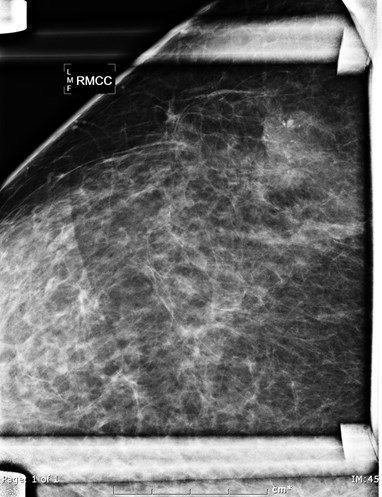
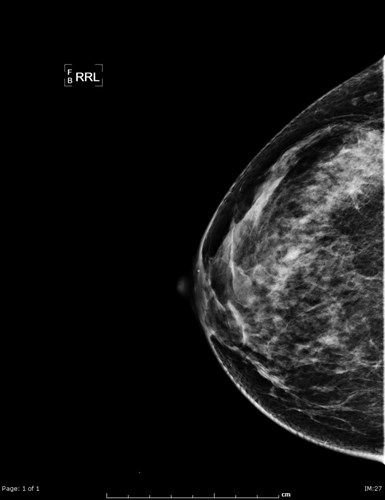
Mammographic Technique: TheCraniocaudal View
•Posterior nipple line-drawn from nipple toback of film or pectoralis (whichever comes1st) should be within 1 cm of pnl on MLO
•Routinely see pectoralis muscle ~30% of time
•Careful not to call medial insertion of thepectoralis a mass
•If anything, CC should include more of themedial tissue

Mammographic Technique
•Low Kvp (~25Kvp) provides excellent contrast
•MAS depends on thickness/density of breast
•Mammography uses Automatic ExposureControl (terminates exposure when sufficientxray photons have reached it)
•Compression: separates tissue, decreasesdose, prevents motion

BIRADS
•Purpose: standardize reports, improvecommunication, audit performance
•Reports must contain:
–Breast tissue type
–Comparisons vs baseline
–Abnormalities
–Impression with final assessment category

BIRADS: Final AssessmentCategories
0 Incomplete: needs additional imaging evaluation
1Negative
2Benign findings
3Probably benign: short term follow uprecommended
4Suspicious abnormality: biopsy should beconsidered
5Highly suggestive of malignancy
6Malignant by biopsy but prior to definitive therapy

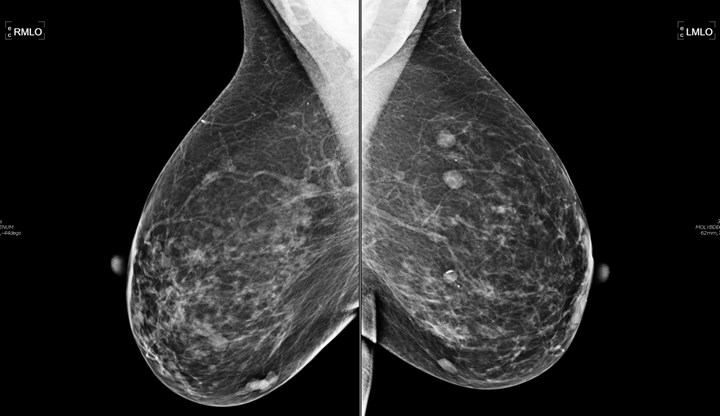
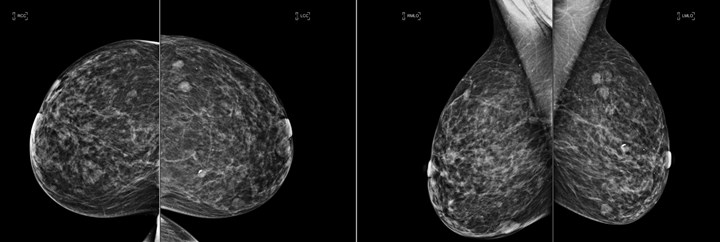
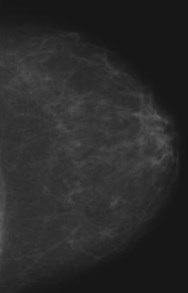
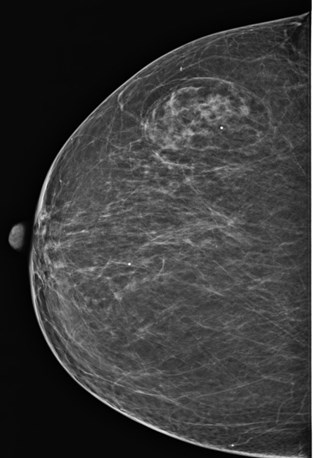
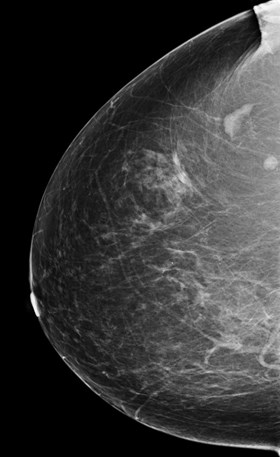
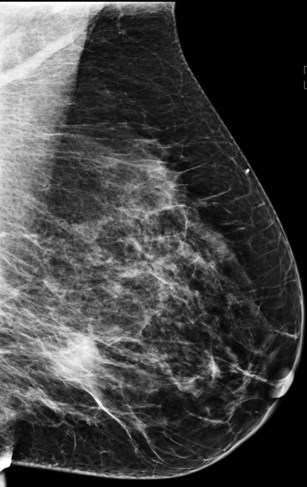
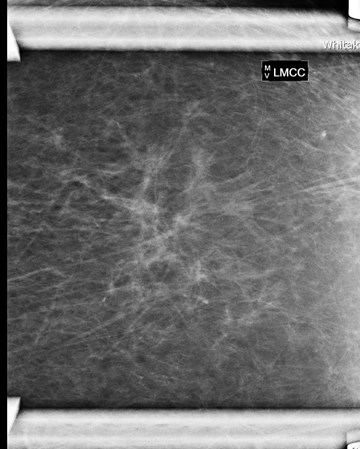
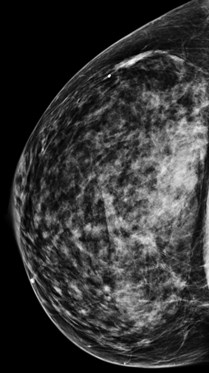
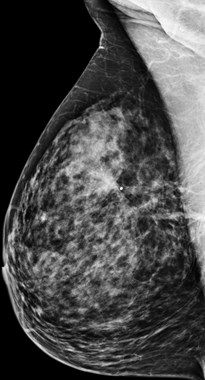
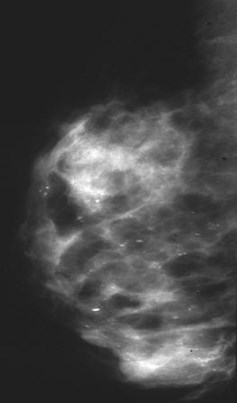
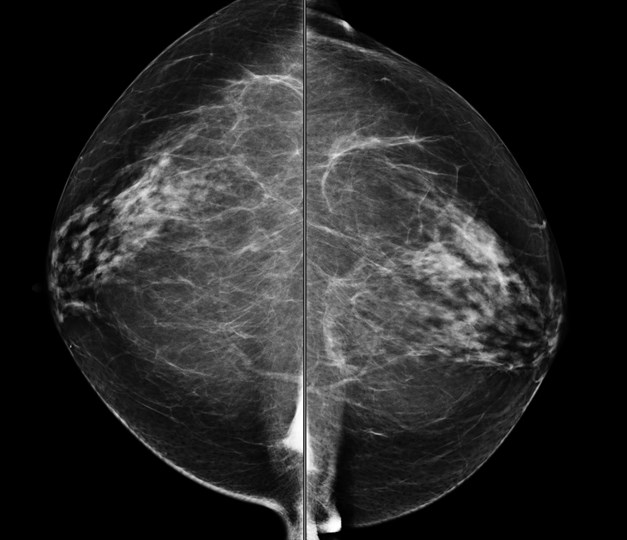
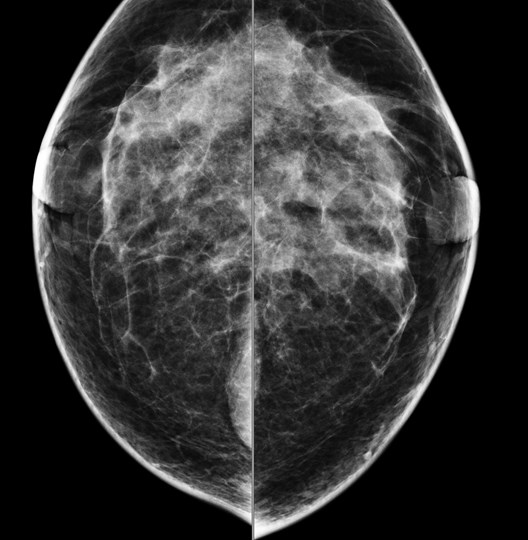
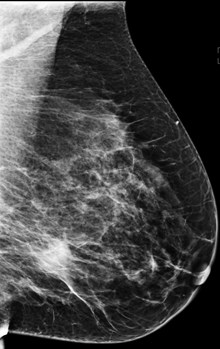
BIRADS Terminology: BreastDensity
•Fatty: < 25 % glandular elements
•Scattered fibroglandular: 25%-50% glandular
•Heteregenously dense: 51%-75% glandular
•Extremely dense: >75% glandular
As of 2014 we do not decide densitybased on percentages!

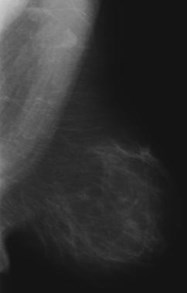
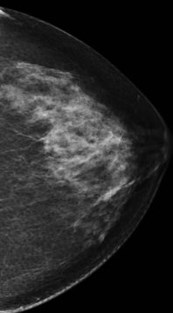
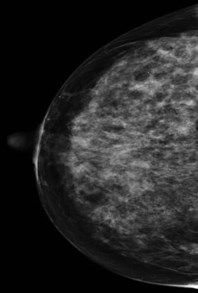
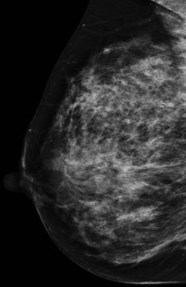
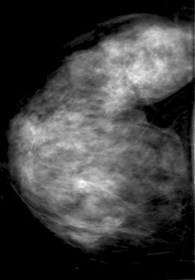
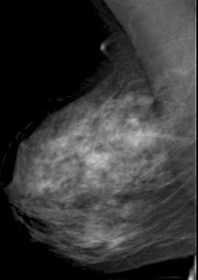
FATTY
SCATTERED
FIBROGLANDULAR
HETEROGENEOUSLY
DENSE
EXTREMELY
DENSE

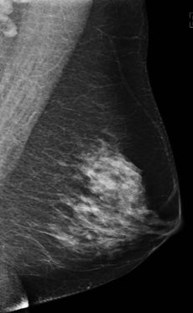
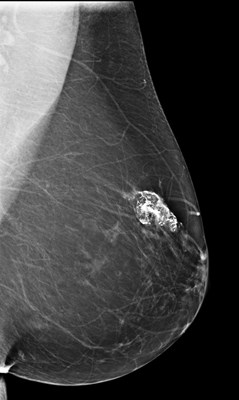
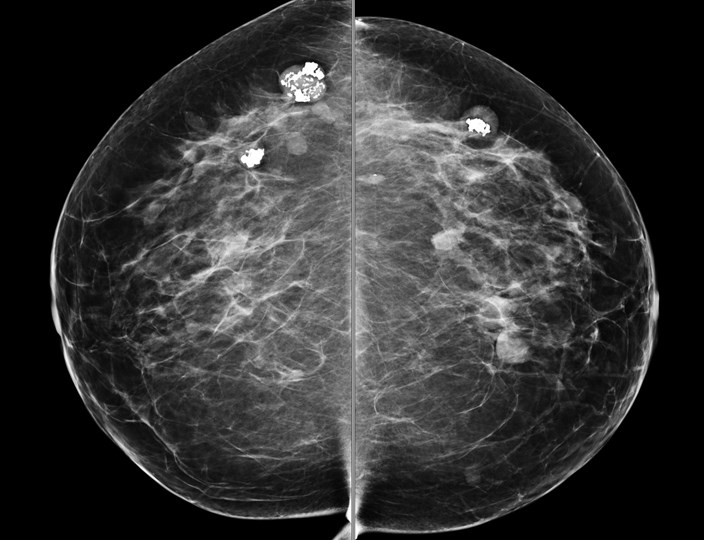
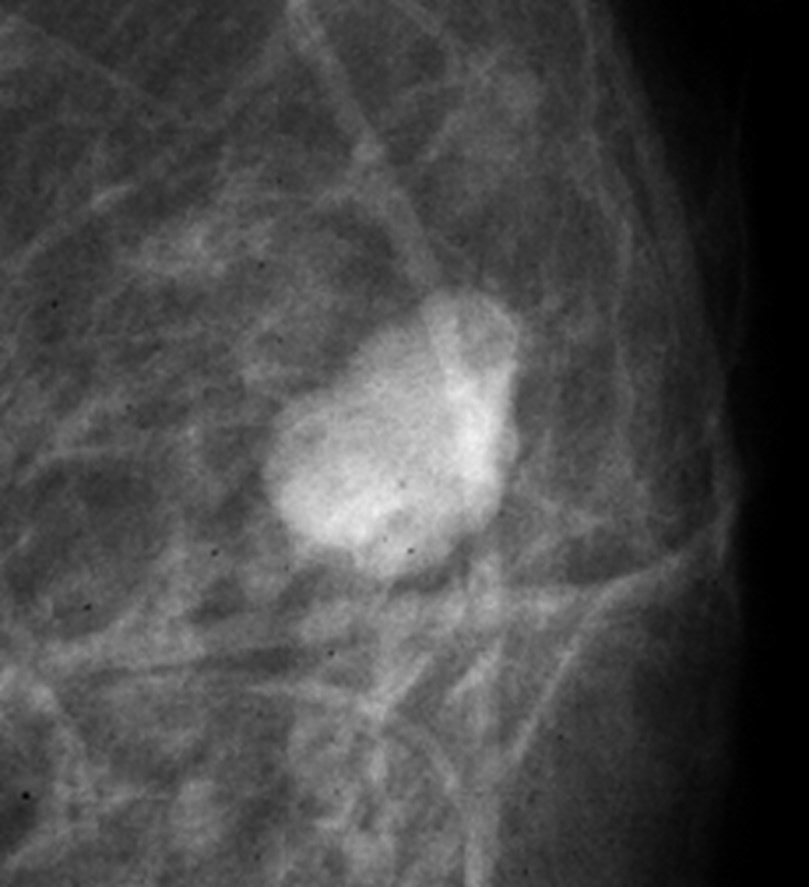
BIRADS Terminology: Breast Masses
•Shape
–Round, oval, lobular, irregular, spiculated
•Margins
–Circumscribed, microlobulated, obscured, indistinct, ill-defined, spiculated
•Density
–High denisty, isodense, low density, fat-containing
•Associated findings
–Skin or nipple retraction, skin thickening, trabecularthickening, axillary adenopathy, architectural distortion

Fat containing masses

Dense, irregular mass with irregular margins

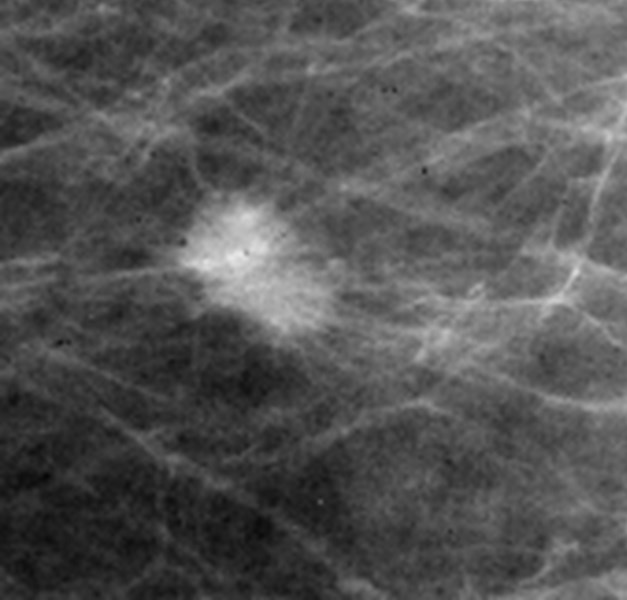
Distortion
Radial scar

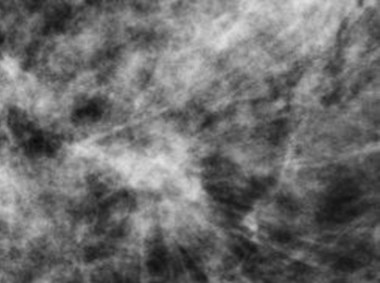
Distortion
Invasive carcinoma

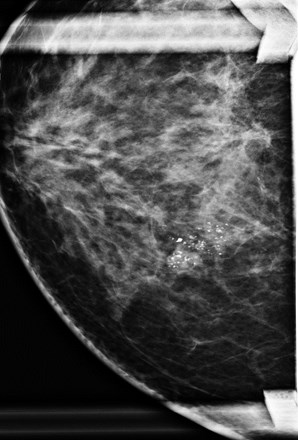
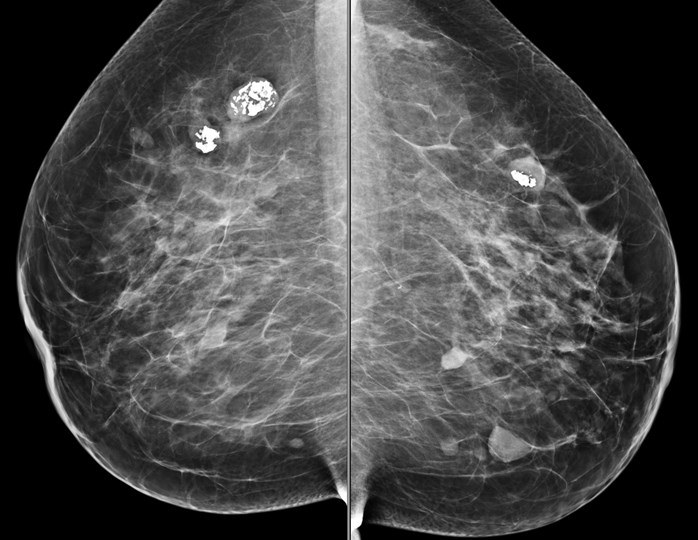
BIRADS Terminology: Calcifications
•Morphology
–Typically benign
•Skin, vascular, coarse or popcorn-like, large rod-like or secretory,round, lucent-centered, eggshell or rim, milk of calcium, suture,dystrophic, punctate
–Intermediate
•Amorphous, indistinct
–Highly suspicious
•Pleomorphic or granular, fine, linear or fine linear branching
•Distribution
–Grouped or clustered, linear, segmental, regional,diffuse, scattered

Benign Calcifications
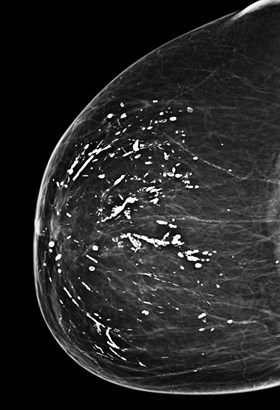

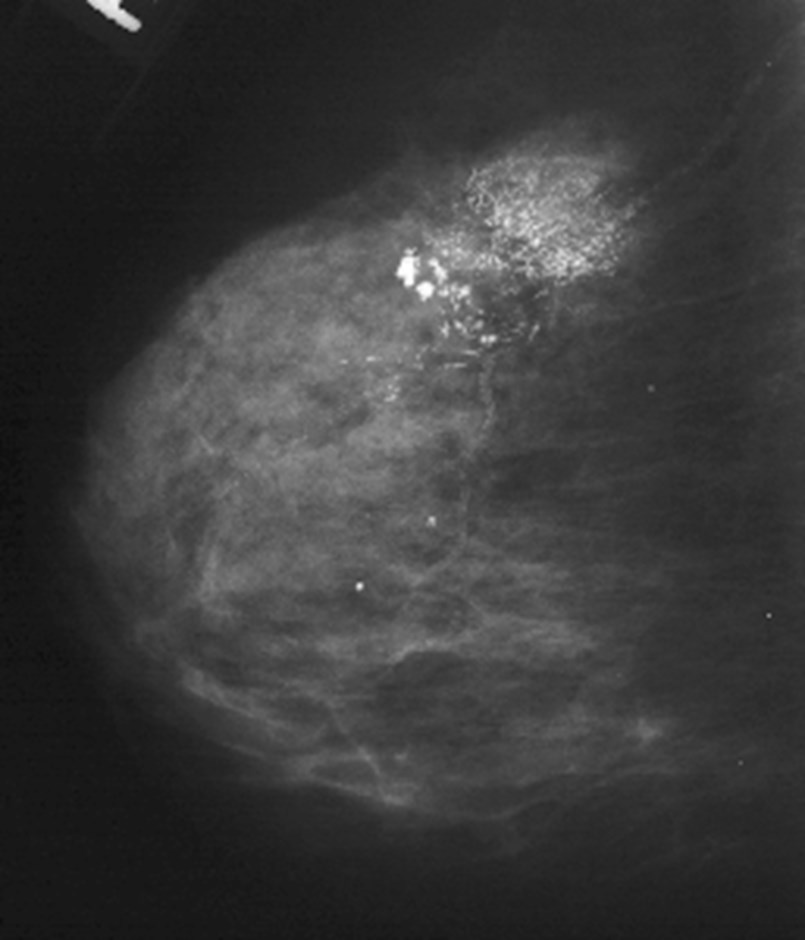
Highly suspicious
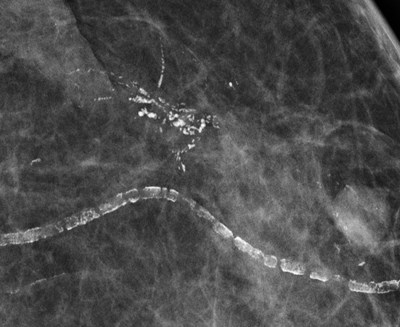
Clustered, pleomorphic
Fine linear branching & casting

What do we look for on amammogram
•4 things: mass, calcifcations, asymmetry,distortion
• Abnormal nodes
•Skin lesions
•Technical problems (motion, inadequate tissue onCC, not enough or concave pec on MLO)

Warning: benign findings/anatomy
•Medial insertion pectoralis
•Sternalis
•Multiple benign masses

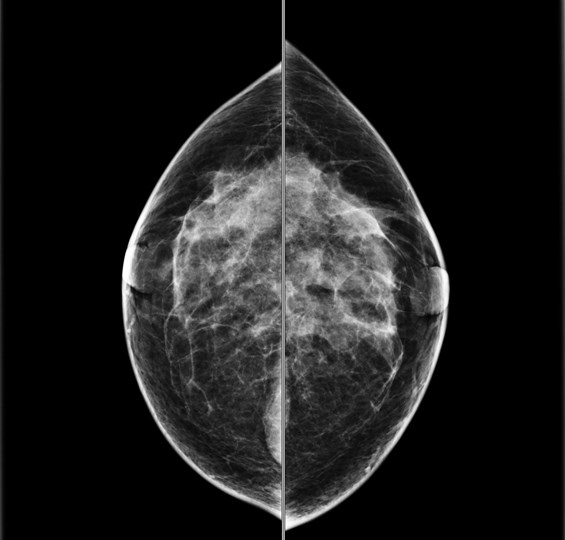
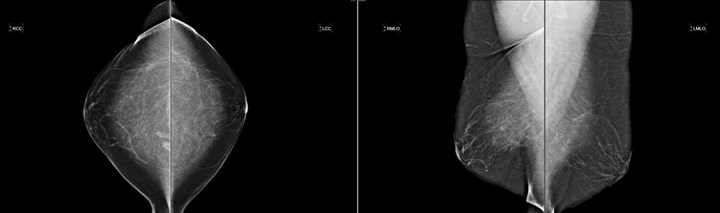
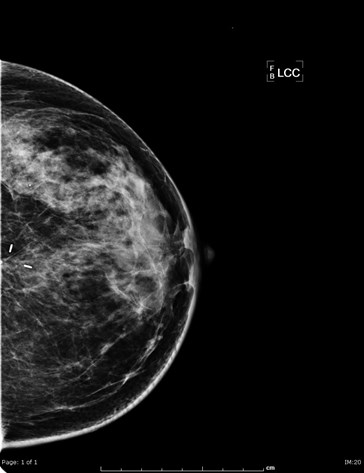
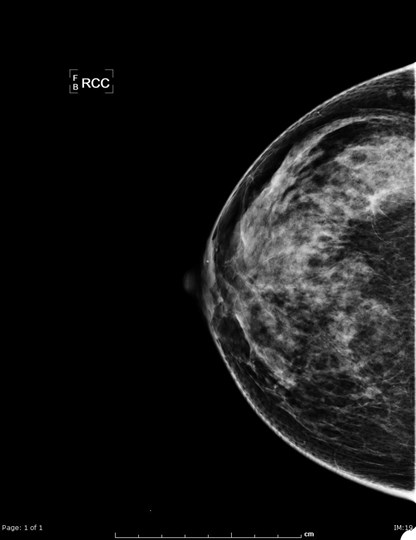
Baseline mammogram
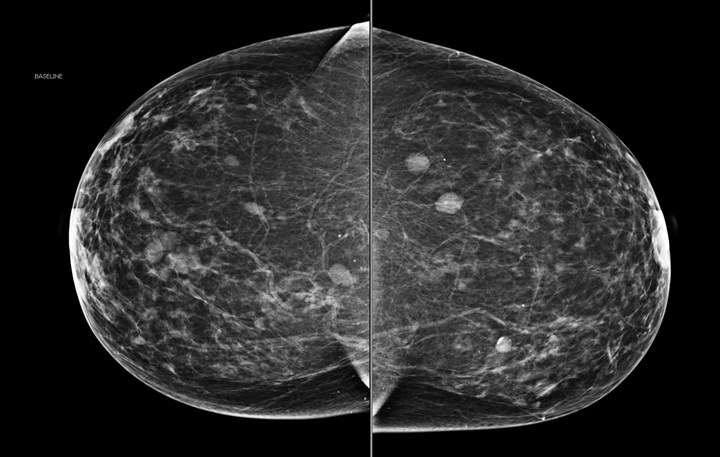

Baseline mammogram
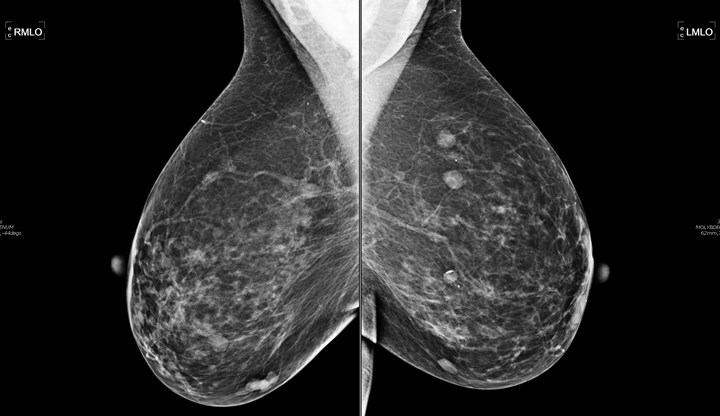

Baseline mammogram







Screening callbacks
•Recall rate: 10% or less
•~95% return to screening (BIRADS 1 or 2)
•~2% 6 month follow up (BIRADS 3)
•<2% have biopsy recommendation (BIRADS 4 OR 5)PPV: 25-40%

Diagnostic Mammography
•Screening callbacks
•Symptomatic patients
•History of breast cancer
•Six month follow up
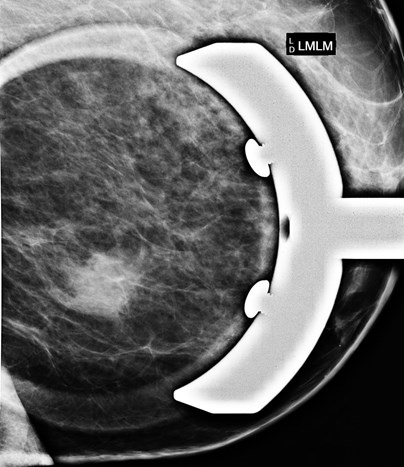
•Implants

Screening Callbacks: Mass
•Spot compression magnification to assessmargins


Screening Callback: Calcifications
•Spot compression magnification in CC andTRUE LATERAL (90)
Baseline mammogram


Screening Callbacks: Where is it?
•If you see something on the MLO but not theCC: TRUE LATERAL (aka lateral or 90 degree)
–If it moves down on the lateral compared with the locationon the mlo, it is in the outer breast
–If it moves up on the lateral, it is in the inner breast

Screening Callbacks: Where is it?
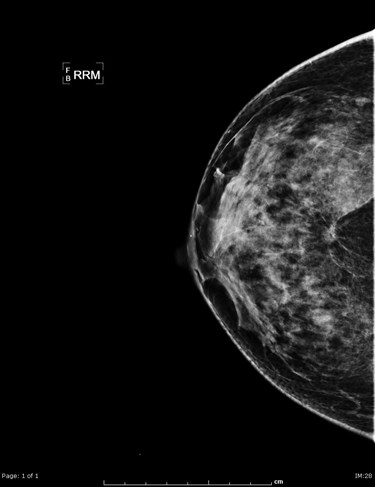
•If you see something on the CC but not on theMLO view: ROLLED VIEWS
–By convention, the tech does a CC view but moves the topof the breast medially (RM) and laterally (RL)
–If the lesion moves medially on the RM and laterally on theRL it is located in the superior breast


Screening Callbacks: Is it real?
•Use spot compression (no magnification) to“press out” possible masses or asymmetry
•Also use true lateral view or rolled views



Thanks for your attention!

Baseline mammogram


Baseline mammogram
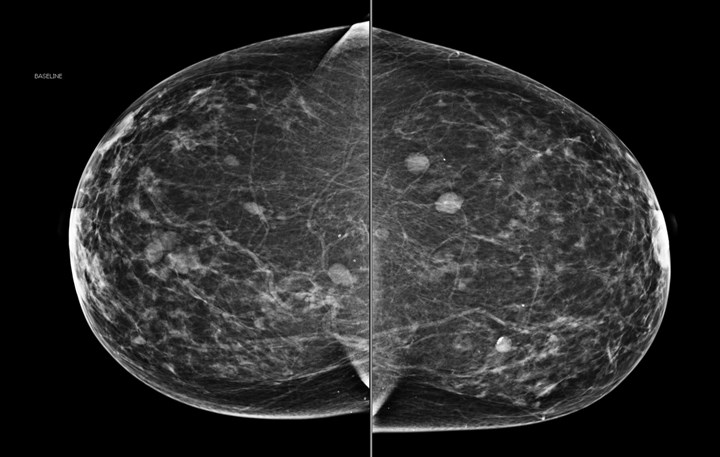

Baseline mammogram